From 3D printing bones to mass producing medicine, nothing has fueled the progress of healthcare more than the innovations of technology. As with all major advances from the wheel to electricity, technology has become interwoven in the infinite facets of our lives.
We can learn a lot about where we’re headed from where we’ve been. As this is such an expansive topic, we’re kicking off the discussion with three of the biggest technological contributions to medicine, and how we’re using them today to make medical care more effective, and more accessible.
3D organs & Robots in the O.R.
First on our list is something straight out of an A.I. Science Fiction movie. Thanks to 3D printing technologies; some internal organs, and even bones can be quickly generated and implanted into the body. 3D printing even makes aids like prosthetics more financially accessible because of lower production costs, and easier manufacturing.
3D tech isn’t just about creating objects, it’s also about mapping. 3D modeling – like the kind used to scan actors for CGI – can be used to map a patient’s insides for better diagnosis, and also used to create a simulated environment for surgeons to test out procedures before taking a solution to the table.
Using 3D mapping in combination with robotic surgeries has had great impact on delicate operations like mitral valve repairs, and spinal surgeries. Robotic surgeons are highly sensitive and specific machines, programmed and operated by advanced medical teams, to carry out extremely delicate procedures with increasing specificity. Imagine, 50 years down the road, what remote operated surgical machines could do for patients with limited mobility, or rural geographies.
Big Data in the Palm of Your Hand
Since we’re already talking about mapping things, we need to zoom in on big data. What is “big data”, just a fancy way of saying a really, really, large amount of data spanning multiple endpoints, (patient age, population, symptoms, finances, medical history, etc.). And we know, it sounds a bit scary.
There’s a stigma around big data that it’s somehow all knowing and therefore invasive – but when it comes to medicine, big data allows for vast intuitive care.
The Healthcare sector’s big data market will reach roughly $70 billion dollars by 2025, according to consulting firm, Bain & Company.
The equation is simple: more data + increased collection speed = an increase in healthcare applications. The biggest hurdle for data – up until now – has been obstacles when it comes to transferring data between medical institutions. HIPAA, security parameters, and legal boundaries all make it challenging for data to be used across organizations to chart and map health trends, predict disease patterns, and analyze health issues for specific populations.
Why Do We Need Data to Be Borderless?
Having secure access to widespread medical data means that organizations can create wellness channels, make informed decisions about where hospitals are needed, see the scope of need for certain therapies, and track trends that affect the overall health of the nation.
But once we have all the data? How can we best implement it at scale?
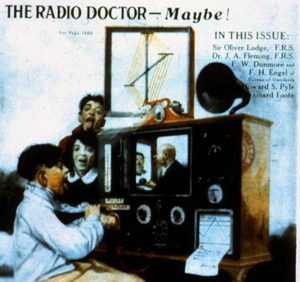
Telehealth
The Mayo Clinic defines Telehealth as:
Telehealth is the use of digital information and communication technologies, such as computers and mobile devices, to access health care services remotely and manage your health care.
With this definition we can apply the word telehealth to anything from calorie counting apps, to remote monitoring for pacemakers. “If you build it, they will come”, and in this digital field of dreams, apps offer infinite solutions to remote healthcare obstacles.
Mobility is an issue for disabled and elderly populations especially, telehealth not only offers medical visits via video – but can also orchestrate transportation and manage insurance and financing.
In conjunction with big data applications, organizations that employ comprehensive telehealth solutions can prioritize patients by risk, constantly evaluate treatments and needs, manage scheduling, prescriptions, administer supportive therapies (physical therapy and psychiatric care), as well as create single-button communication pathways between patient and practitioner.
Data = Data
By increasing care accessibility to patients, we increase their willingness to participate in their care journeys. More data equals more resources and more information which can be analyzed for further care programs and medical advances.
Complex Architecture for Better Health
Creating a smart architecture is step one to implementing and assessing the benefits of big data, and applying it to a telehealth solution. In recent years, the Primavera team has mapped and constructed its architecture along with developing technologies.
Through the pairing of a complex IT architecture with relationship database systems, the primavera team has focussed on contributing to closing the information gap when it comes to healthcare data resources.
Our system stands out as one developed by working practitioners alongside top-tier developers and healthcare executives to revolutionize the practical application of data and apply it to care continuum advancements.
A stand-alone operating system, Primavera is incredibly simple to use for both patients and practitioners. Designed for efficiency, and packed with the clinical and financial tools needed to run your practice.
Medical technologies and data applications will only continue to advance. You want to partner with a platform that can grow along with tech while prioritizing patients and the success of your practice. It’s easier together. Reach out to us today for a demo.

















Recent Comments